Awareness Is Rising, Access Isn’t: Mental Health in Texas, 2025
Mental health is no longer a background conversation in Texas. In 2025, it has become central—influencing legislation, shaping public discourse, and straining core infrastructure: schools, hospitals, and correctional facilities.
Texas has made significant moves: in 2023, the state approved a record $11.68 billion in behavioral health funding—the largest investment in its history.
And yet, for many Texans, care remains out of reach.
In recent surveys, 41% of residents said they or someone they love needs mental health support but can’t access it. The top barriers? Cost, confusion, and a shortage of providers (Ipsos, 2023; Statesman, 2025).
Stigma is fading. Public awareness is rising. But the system still struggles to respond. More Texans than ever are willing to seek help—but too often, they don’t know where to begin.
Access and Structural Barriers
In Texas, access to mental health care depends on where you live, what coverage you have, and whether a provider is available.
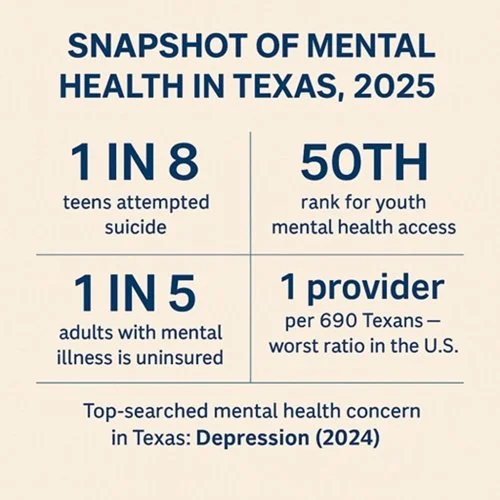
As of 2022, 98% of Texas counties reported mental health workforce shortages. More than 88% of Texans live in these shortage areas, and statewide, the ratio averages one provider for every 690 residents—the worst in the country (Health Resources and Services Administration, 2022).
Among youth, the gap is even starker. Texas has just 10 child and adolescent psychiatrists per 100,000 youth, compared to the recommended 47. The result? Texas ranks 50th in the nation for youth mental health access.
Insurance compounds the issue. Texas leads the country in uninsured rates; more than 1 in 5 adults with mental illness lacks coverage.
While stigma is fading, the system remains fragmented. Texans often describe it as confusing, costly, or simply out of reach. In rural areas, care may be limited to emergency rooms or law enforcement.
And despite rising awareness, the gaps remain stark. In 2024, depression was the most-searched mental health concern in Texas (Google Trends, 2024)—yet more than 75% of youth with major depression receive no treatment (Mental Health America, 2024).
Accessing care shouldn’t compound the seeker’s distress.
Youth Mental Health: A System in Strain
Youth mental health doesn’t exist in isolation. It intersects with education, crisis care, and family systems—and in Texas, those systems are under pressure.
By 2021, 47% of Texas high school students reported persistent sadness or hopelessness. 1 in 5 seriously considered suicide; 1 in 8 attempted it. Among adolescent girls, attempts rose 51% in two years (CDC, 2021; Texas Department of State Health Services, 2021).
This isn’t new. It’s a long-building crisis now too visible to ignore.
School-based services are overextended. Some counselors cover multiple campuses, serving 800 students or more. Even when crises are recognized, follow-up care is often unavailable.
Emergency rooms have become default entry points. But ERs are built for triage, not recovery. Students return to environments unequipped to support them.
Stressors like trauma, academic pressure, and social isolation remain common. Programs like Texas Child Health Access Through Telemedicine (TCHATT) have expanded school-based care, but coverage is still uneven—especially in under-resourced areas.
Without earlier intervention and sustained care, schools will remain overburdened—and students at risk.
Recognition Without Direction: Diagnosis Doesn’t Guarantee Care
Recognition is rising—but response still lags behind.
Between 2016 and 2020, Texas saw a 29% increase in anxiety diagnoses and a 27% increase in depression diagnoses among children (Texas Department of State Health Services, 2021). Adult diagnoses of ADHD and autism are also growing—especially among women, late-identified adults, and others historically overlooked.
This isn’t overdiagnosis. It’s progress. What was once dismissed as moodiness or disorganization is now recognized as emotional dysregulation, sensory overload, or executive dysfunction. Many are finding the language—and the community—that once felt out of reach.
But diagnosis is only the beginning.
Texans newly diagnosed with ADHD or autism often struggle to find providers trained in neurodivergent-affirming care. Meanwhile, demand continues to grow, waitlists stretch, and local options remain limited—leaving many to navigate the system on their own.
Trauma and Substance Use: Overlapping Realities
Mental health doesn’t stand alone. It’s shaped by trauma, instability, and increasingly, by addiction.
In Texas, nearly 1 in 5 children has experienced multiple Adverse Childhood Experiences (ACEs), and nearly half have experienced at least one (Child Trends, 2021). These early adversities are strongly linked to later risks of depression, anxiety, suicidality, and substance use.
Meanwhile, overdose deaths are surging. In Travis County, fatalities tripled between 2019 and 2023. Fentanyl was involved in nearly half of all overdose deaths statewide by 2022 (Texas Health and Human Services Commission, 2024).
These aren’t separate crises—they’re overlapping.
Clinics report rising cases of co-occurring conditions: PTSD with methamphetamine use, anxiety with opioid misuse, depression with alcohol dependence.
Yet care systems remain siloed. Few programs offer trauma-informed, harm-reduction, and medication-assisted treatment in one place, making integrated recovery challenging for many Texans.
Community-Based Solutions in Central Texas
While access remains limited across much of the state, several Central Texas programs offer working examples of early, embedded care:
Integral Care’s Therapeutic Diversion Center provides 24/7 crisis stabilization as an alternative to incarceration or the ER—reducing strain on emergency systems and offering short-term support (Integral Care, 2024).
Bluebonnet Trails operates youth respite and justice system-based mental health restoration programs, diverting children and adults from hospitalization or prolonged incarceration (Bluebonnet Trails Community Services, 2024).
Austin Child Guidance Center offers walk-in therapy, sliding-scale services, and bilingual assessments—making care accessible regardless of income or insurance (Austin Child Guidance Center, 2024).
CPAN and TCHATT, through Dell Medical School, provide psychiatric consultation and school-based teletherapy to 13 counties—partnering with pediatricians and school counselors to support students before crises escalate (Dell Medical School, 2024).
These programs show what’s possible when care is local, coordinated, and designed toward early intervention.
State Investment and Workforce Innovation
In 2023, Texas approved $11.68 billion in behavioral health funding—the largest in state history (Meadows Mental Health Policy Institute, 2024). Key allocations included:
These investments are significant. But funding alone doesn’t guarantee access. Without Medicaid expansion, stronger parity enforcement, or long-term workforce support, even well-designed systems may go underused.
To expand provider reach, Texas is moving to join the Interstate Counseling Compact, which would allow licensed counselors to practice across state lines. In 2025, bills HB 1537 and SB 498 were introduced with backing from the state licensing board (Texas Legislature Online, 2025; Texas Behavioral Health Executive Council, 2023).
Texas is investing. But in a system marked by fragmentation, whether that investment translates to care remains to be seen.
Looking Ahead
Texans are more open to help than ever before. But access still depends on where you live, what you earn, and who you are.
The state is investing. Local programs show what’s possible. Workforce efforts like the Counseling Compact offer promise—but funding doesn’t guarantee reach, and recognition doesn’t ensure support.
Texas is building. But the road from recognition to care remains unfinished.
References
Austin Child Guidance Center. (2024). Walk-in clinic services. https://www.austinchildguidance.org/what-we-do/our-services/walk-in-clinic.html
Bluebonnet Trails Community Services. (2024). Behavioral health services and programs. https://bbtrails.org
Centers for Disease Control and Prevention. (2021). Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic — United States, January 2019–May 2021. Morbidity and Mortality Weekly Report, 70(24), 888–894. https://doi.org/10.15585/mmwr.mm7024e1
Child Trends. (2021). Adverse childhood experiences: National and state-level prevalence. https://www.childtrends.org/publications/prevalence-of-adverse-childhood-experiences-national-and-state-level
Dell Medical School. (2024). Child Psychiatry Access Network (CPAN) and TCHATT programs. University of Texas at Austin. https://dellmed.utexas.edu/units/department-of-psychiatry/cpan-tchatt
Google Trends. (2024). Mental health search trends by U.S. state. https://trends.google.com/trends/
Health Resources and Services Administration. (2022). Health professional shortage areas (HPSA) – Mental health care, Texas. U.S. Department of Health and Human Services. https://data.hrsa.gov/topics/health-workforce/shortage-areas
Integral Care. (2024). Therapeutic Diversion Center: Reducing incarceration through mental health stabilization. https://integralcare.org
Ipsos. (2023). World Mental Health Day 2023: U.S. findings. https://www.ipsos.com/en-us/ipsos-world-mental-health-day-report
Meadows Mental Health Policy Institute. (2024). 88th Texas Legislature wrap-up: Mental health investments. https://mmhpi.org/policy/88th-texas-legislature-regular-session-wrap-up/
Mental Health America. (2024). The state of mental health in America 2024. https://www.mhanational.org/issues/state-mental-health-america
Statesman. (2025, May 15). Mental health awareness month highlights barriers for Texans. Austin American-Statesman. https://www.statesman.com/story/news/state/2025/05/15/mental-health-awareness-month-mental-illness-challenges-texas-americans-survey/83627192007
Texas Behavioral Health Executive Council. (2023). Board news and updates. https://bhec.texas.gov/texas-state-board-of-examiners-of-professional-counselors/board-news/
Texas Department of State Health Services. (2021). Texas youth risk behavior surveillance system (YRBS) results. https://www.dshs.texas.gov/maternal-child-health/adolescent-health
Texas Health and Human Services Commission. (2024). Texas opioid overdose data and trends. https://www.hhs.texas.gov/about-hhs/records-statistics/data-statistics/opioid-data
Texas Legislature Online. (2025). HB 1537 Bill text. https://capitol.texas.gov/BillLookup/Text.aspx?LegSess=89R&Bill=HB1537
Texas Legislature Online. (2025). SB 498 Bill text. https://capitol.texas.gov/BillLookup/Text.aspx?LegSess=89R&Bill=SB498
The Daily Texan. (2024, June 10). New Austin State Hospital opens in partnership with Dell Medical School. https://thedailytexan.com/2024/06/10/new-austin-state-hospital-opens-in-partnership-with-dell-medical-school/